When you are living with type one diabetes, insulin is probably the hormone you think about the most. With so much mental energy dedicated to managing this one hormone, it can be easy to forget that other hormones can impact blood sugar levels too.
While many hormone patterns in men tend to follow a roughly 24-hour rhythm, a women’s hormone cycle, also known as the menstrual cycle, typically lasts 21-38 days. This longer, more complex cycle can make it harder to understand how hormonal changes affect blood sugar levels.
Before we can explore the potential connection between the menstrual cycle and diabetes, let’s take a closer look at how the menstrual cycle works.
What is the menstrual cycle?
The menstrual cycle is often described as having two main phases, starting with the follicular phase. This phase begins on the first day of menstruation (your period) and ends at ovulation. During this time, an egg matures in the ovaries.
Ovulation occurs between the two phases. It is a short window, typically lasting 12 to 24 hours, where the ovary releases an egg. While ovulation typically occurs about 14 days before the next period, the exact timing can vary from person to person and cycle to cycle.
After ovulation, the luteal phase begins and usually lasts around 14 days. During this phase, the body produces progesterone to support a potential pregnancy. If pregnancy does not occur, hormone levels drop, the uterine lining sheds, and a new menstrual cycle begins.
Does the menstrual cycle impact blood sugar levels?
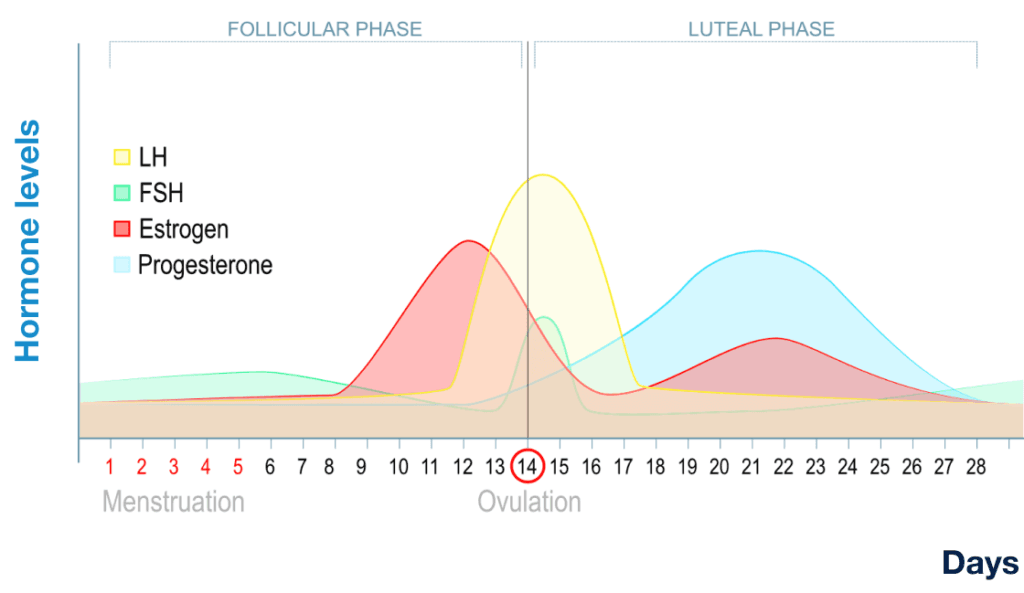
A number of hormones fluctuate across the menstrual cycle, and these changes can influence insulin sensitivity. At the start of your period, progesterone and estrogen levels drop. Many people report becoming more sensitive to insulin and needing less insulin during this time. Insulin requirements often shift again after the first few days of menstruation and may remain closer to baseline through the follicular phase.
Around ovulation, there is a surge in luteinizing hormone (LH), triggering the release of an egg. Some people experience increased insulin resistance around this time or in the days leading up to ovulation, though responses vary widely.
After ovulation, during the luteal phase, progesterone levels rise and remain elevated until the next period. Many people find they require more insulin around 3-7 days prior to the start of a period, but individual patterns can differ from cycle to cycle.
It’s important to note that while these patterns are commonly reported, research findings are mixed. Some published studies have not detected statistically significant differences in average blood glucose across cycle phases, and the science is still developing.
To help close these research gaps, organizations like Tidepool have launched initiatives such as the Tidepool Period Project. In 2025, Tidepool announced a partnership with Oura to further investigate how menstrual cycles affect blood sugar and insulin needs in people with diabetes.
How can Gluroo help you understand your menstrual cycle?
The first step in answering this question is understanding your own body. While the research is sparse and inconclusive, one thing is clear: every body is different. Hormonal responses can also change over time, so it is normal for your diabetes experience to look different during puberty, adulthood, pregnancy, or menopause.
One of the most effective ways to understand your personal patterns is to log both your blood sugar data and your menstrual cycle. Once you have this information, it is important to look for trends. Check if your blood sugar levels or insulin requirements are increasing at certain phases of your cycle.
Having all of this data in one place can make these patterns easier to spot. In Gluroo’s new menstrual tracking feature, users can log their periods. You can overlay this period data with your blood sugar, insulin, and carbs over the past 7-90 days to see how they may be connected.
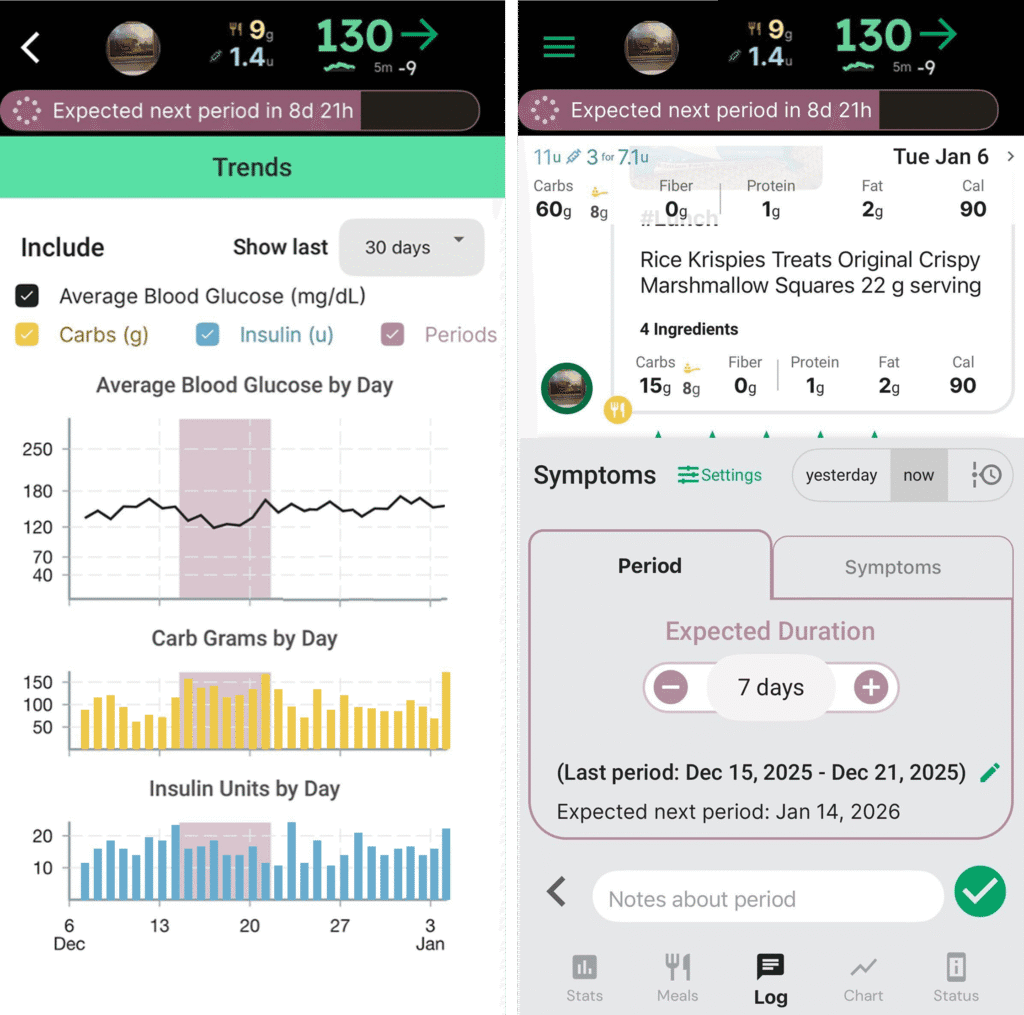
After tracking two or three cycles, you may begin to notice early trends. Because hormone levels and insulin sensitivity can vary from cycle to cycle, patterns become more reliable as more data is collected over time.
Once you’ve identified patterns, the next step is preparation. For example, if you notice increased insulin resistance in the week leading up to your period, you can plan ahead by setting reminders and adjusting expectations so you’re not left wondering why your insulin seems less effective. Gluroo allows users to set reminders based on predicted cycle timing, helping to reduce surprises.
There are many factors that influence blood sugar levels; sometimes a CGM can feel more like a random number generator. But gaining a better understanding of how key pieces of this puzzle, such as your menstrual cycle, affect your blood sugar levels can help make sense of it all. While there’s no perfection in diabetes, taking the time to log and learn about yourself can really help to simplify diabetes.
