Type 1 Diabetes is a chronic condition in which the pancreas produces little to no insulin. It can be extremely challenging for adults to manage, not to mention children who may not yet have the skills or understanding to recognize and address their symptoms. As a teacher, it’s important to be aware of the condition and to know how to help your students in an emergency or in general. In this article, we’re going to take a look at some of the most useful tips and tricks for helping out students in your classroom that have T1D and present the ultimate teachers guide to type 1 diabetes.
What is Type 1 Diabetes?
On a very high level, Type 1 Diabetes is an autoimmune disease in which the immune system attacks the cells in the pancreas that produce insulin. Insulin is a hormone that helps regulate blood sugar levels. Without insulin, the body cannot properly use the energy from food, leading to high blood sugar levels. High blood sugar over many years can cause significant problems such as blindness. Extremely high blood sugar, even for only several hours, can cause organs to begin to fail and require immediate medical attention.
A Type 1 Diabetic (T1D) will need to actively manage their blood sugar levels by taking insulin (decreasing blood sugar) and eating carbohydrates (increasing blood sugar) to keep their blood sugar in a target range. A T1D will have a device that lets them check their blood sugar levels, either by drawing blood from a fingertip or via a sensor attached to their body. They will also have a device for administering insulin – either by injecting it themselves with insulin pens and needles, or another device attached to their body called an insulin pump that can give insulin automatically. It’s important that the T1D is able to keep these devices accessible to them at all times.
Communicating With Parents And Other Staff
All T1D students should have some sort of emergency plan submitted to the school nurse(s). This is covered in a 504 health plan – a “legal, written document specifying what “reasonable” modifications and accommodations the school must provide for a student with a disability.” As a teacher, you may want to be included in this plan, at the very least so that you know what is and is not expected of you in the event of an emergency. To be clear, section 504 is a federal civil rights law. Different states and school districts will have their own processes around managing it.
The best practice is to have an open dialogue between the school administration, teachers, nurses, and parents. For this reason, you should have a meeting at the start of the year with all of the above to discuss how things should be handled by each party.
Hypoglycemia
Type 1 Diabetics must manage their blood sugar by administering insulin, usually via injections with a pen needle or with a pump that is attached to their body at all times. One of the acute dangers of this disease is when you administer too much insulin, causing blood sugar levels to drop too far. This is called hypoglycemia, and severe cases can result in unconsciousness or even death. Minor cases of hypoglycemia may happen frequently, since the amount of insulin to inject depends on estimates of the carbohydrate content of foods that the T1D consumes. It is very easy to misjudge.
As a teacher, you’re not expected to be helping the child manage their diabetes at every second of every day. One of the best ways you can help, though, is to be aware of the signs of severe hypoglycemia and how to address it.
How to Recognize and Address Hypoglycemia
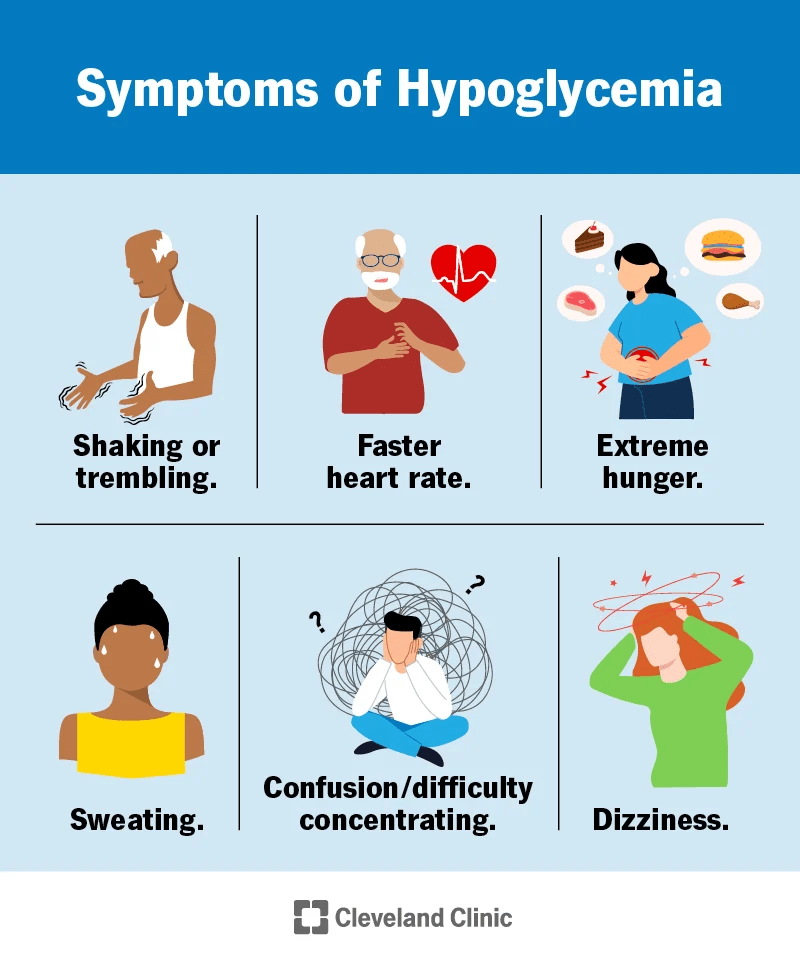
Hypoglycemia, or low blood sugar, is a common complication of Type 1 Diabetes. Symptoms of hypoglycemia can include shakiness, dizziness, confusion, irritability, and sweating.
If you notice a T1D student exhibiting any of the symptoms above, you should first alert the school nurse so that they’re aware of the situation. Then, it may be helpful to quickly check in with the student to see how they’re feeling. For example, you could ask them what their blood sugar level is. They may be wearing a CGM, in which case they would have a phone or other small device that shows blood glucose readings from the CGM. As a general rule of thumb for children, any number below 70 mg/dL (or 4.4 mmol/l) may be of concern. If they don’t have a CGM, then maybe they have a finger-prick blood glucose meter. In this case, they will be able to check their blood glucose reading by drawing a small amount of blood from a fingertip.
It’s important to note that this is just a general guideline. The 504 plan that you discuss with the student’s parents and school nurses may have specific details that are different than those outlined here. For example, some parents may prefer that you not intervene until the T1D’s blood glucose level is below 65 mg/dL. Others might want anything under 85 treated.
Emergency Supplies to Keep
Regardless of the types of devices they use for managing diabetes, the treatment for low blood sugar is the same – eat fast-acting carbohydrates. This includes things like glucose tablets, glucose powder, sugary candies like smarties and fruit snacks, or juices like orange and apple juice. It’s a good idea to have some of these things on hand in your classroom in case a student runs out of their own supplies. Note that most sugar-free snacks do not work to raise blood sugar levels.
Ultimately, the responsibility for addressing the “hypo” is on the student and the school nurses, not you. You should never force a student to eat something or take any action to manage their diabetes. It’s such a complex topic that you cannot be expected to understand it by reading one article on the web. In summary, here’s what you can be prepared to do to help out if you think they’re experiencing hypoglycemia:
- Have sugary snacks available in your classroom. As before: glucose tablets, glucose powder, sugary candies like smarties and fruit snacks, or juices like orange and apple juice
- Make sure a school nurse is aware of the situation
- Offer to help the student by walking with them to the nurses office. Or, send a buddy with them to escort them. Most 504 plans will require that the T1D with hypoglycemia is not left alone at all, even for a moment.
How Should You Approach Diabetes In The Classroom?
Type 1 Diabetes can be a very touchy subject. Families differ widely in how they want school staff and faculty to intervene in their child’s diabetes management. Some families want to let everyone know that their child has diabetes. Others will prefer to keep it as quiet as possible. Diabetes can be a very alienating and socially painful experience for some children (speaking from experience). You should be very careful when bringing attention to a student’s diabetes for this reason. You should also never share information about the student’s disease without explicit permission from the child and/or their parents.
Access to Smartphones or Other Devices

Many Type 1 Diabetics require a smartphone to be on them at almost all times. The smartphone may connect to their insulin pump, insulin pen, continuous glucose monitor (CGM), and/or finger prick reader. These devices may cause the phone to give off loud alerts, alarms, or vibrations to signal to the student that their blood sugar needs attention. For example, the Dexcom G6 smartphone app has some alerts that are unable to be turned off. This is enforced by law through compliance with rules from the U.S. Food and Drug Administration (FDA). For this reason, you should be extra careful when reprimanding a student for checking their phone or interrupting class with a loud alarm. There could be a very legitimate reason for that to happen.
Other kids may use a smartwatch that can show their blood glucose numbers. This approach can be less disruptive than having to pull out and unlock a smartphone.
Gluroo for Diabetes Management
When a T1D student does pull out their phone, it could be to check on any number of apps related to diabetes. One app that aims to reduce the stress of diabetes management for the entire family is called Gluroo.
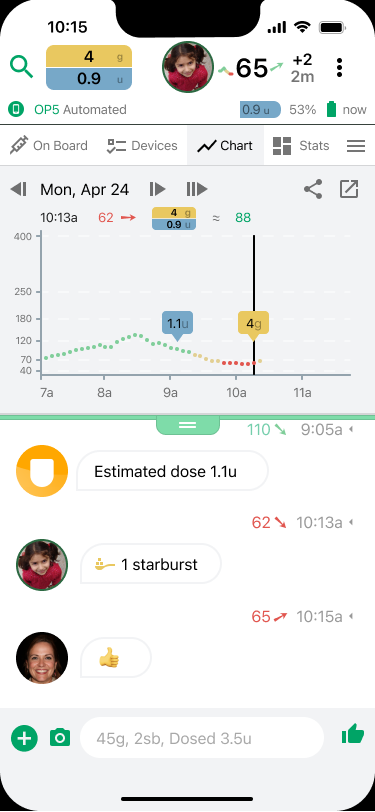
Gluroo is particularly helpful for teachers and other school staff. It enables direct contact between the parents and child at all times. Gluroo provides streamlined group-chat messaging, blood glucose and insulin levels, exercise, device health and more – all in one place for everyone to see. The image above demonstrates a child with T1D having a hypoglycemia event at about 10:00 AM. The child responds on their own by eating a starburst candy and logging it in the app at 10:13 AM. This also notifies the parents. Then, the mother responds with a thumbs up at 10:15 AM. The parents are then able to see that the child has things under control. They also seethat their blood glucose level is trending upwards.
Teachers may rest easier knowing that a student using Gluroo is being monitored at all times by their parents, school nurses, or whoever else the family wants to include in their GluCrew. You can try Gluroo today for free by tapping one of the buttons below.
The Role of Teachers in T1D
Type 1 Diabetes is a very complicated disease. As a teacher, you’re not expected to help the student manage their day to day needs. In fact, that is explicitly the job of the student and the school nurses. What you can do to help, though, is to have emergency supplies on hand, to be able to recognize signs of hypoglycemia, and to adopt an attitude of understanding an empathy when you’re working with a T1D student.

